Abstract
INTRODUCTION: Recent observational studies have revealed that real-world complications of intensive chemotherapy for frontline treatment of acute myeloid leukemia (AML) far exceed those reported in clinical trials. A 2017 analysis of over 40,000 AML patients found that 26% of patients who received induction chemotherapy were admitted to the intensive care unit (ICU), with increased mortality for non-white patients (Halpern, JAMA Oncology 2016). In a newly created Chicago AML registry (Abraham, Blood 2022), higher ICU admission rate was noted following induction chemotherapy for non-white patients. The current study aims to i) describe treatment complications based on race/ethnicity and ii) examine structural racism (SR) measures as risk factors for ICU admission following intensive chemotherapy in a diverse real-world patient population.
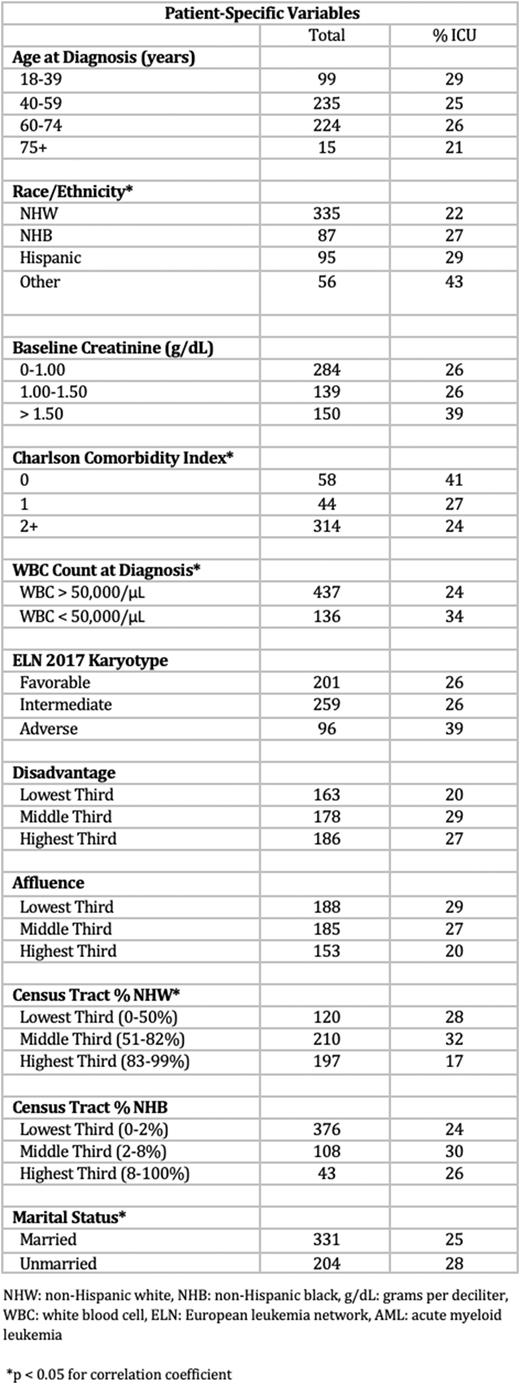
METHODS: Using the Chicago AML registry, we compared ethnoracial differences in treatment complications including infections, thrombosis, renal or liver dysfunction (defined as peak creatinine >1.5 g/dL or peak bilirubin >1.2 mg/dL), respiratory failure requiring ventilatory support and hemodynamic instability needing pressor support. We then examined associations of race/ethnicity and previously published measures of census tract disadvantage, affluence, and segregation (referred to as SR measures) with ICU admission. These structural barriers were examined alongside known predictors of treatment mortality including disease characteristics and comorbidities. Additional outcomes included duration of ICU stay and mortality.
RESULTS: In this cohort of 573 patients who underwent intensive induction chemotherapy for AML, 30-day complications differed based on race/ethnicity. Renal dysfunction was highest in non-Hispanic black (NHB) patients with an incidence of 27.8% with 6% initiating dialysis compared to 17.6% of non-Hispanic white (NHW) and 11.3% of Hispanic patients with 2% needing dialysis. Hepatotoxicity was highest in Hispanic patients (64%) vs. NHB (51%) and NHW (47%). Infectious complications were highest in NHB with microbiologically documented infections in 50.6% compared to 39.7% in NHW and 32.6% in Hispanic. Venous thrombosis occurred in 14.5% of NHB patients, compared to 14.7% of NHW and 13.3% Hispanic patients.
In total, 141 (24.6%) patients required ICU admission during intensive induction with rates differing significantly by race and ethnicity (p = 0.014). Average length of stay in the ICU was 7.8 days for NHB patients, 6.7 days for NHW and 6.0 days for Hispanics. Due to low 30-day mortality, we were unable to detect differences between ethnoracial groups. Mechanical ventilation was utilized in 32% of NHB compared to 26% of NHW and 20% of Hispanic patients admitted to the ICU. Vasopressor were required in 31% of NHB patients vs. 27% of NHW patients.
Predictors of ICU admission in our dataset included non-white race, unmarried status, living in a neighborhood with lower % of NHW residents, and WBC > 50,000/µL at diagnosis. Additional census tract variables including higher disadvantage and lower affluence conferred nonsignificant risk. Interestingly, comorbidities, ELN Score and baseline creatinine > 1.5 g/dL were not predictors of ICU admission.
CONCLUSIONS: In a real-world population of AML patients, we show variation in the spectrum of treatment complications based on race/ethnicity. Moreover, with detailed individual and neighborhood socioeconomic position (SEP) data, measures of SR predicted ICU admission following induction chemotherapy. Other significant predictors include marital status - an individual measure of SEP, and hyperleukocytosis, which may indicate delay in medical presentation. High comorbidity index did not predict increased rate of ICU admission similar to prior studies (Tawfik, J Geriatr Oncol, 2016), while renal dysfunction was a non-significant predictor. Collectively our results suggest that there is a need to incorporate individual and neighborhood SR measures to identify patients at risk of clinical decline when stressed with intensive therapies. An algorithmic approach to identify 'high risk’ patients based on clinical/molecular and structural factors could prompt more detailed assessment of fitness prior to initiation of chemotherapy and directly influence leukemia outcome disparities.
Disclosures
Patel:Kronos Bio: Research Funding; Pfizer: Research Funding; Servier/Agios: Research Funding; Celgene/BMS: Research Funding; AbbVie: Consultancy. Tsai:Jazz Pharmaceutical: Speakers Bureau; Bristol-Myer Squibb: Speakers Bureau. Stock:Kite: Honoraria; Jazz Pharmaceuticals: Honoraria; Pluristem: Consultancy, Honoraria; Kura Oncology: Honoraria; MorphoSys: Honoraria; Pfizer: Consultancy, Honoraria, Research Funding; Amgen: Honoraria; Servier: Honoraria; Syndax: Consultancy, Honoraria; Newave Pharmaceuticals: Consultancy; Agios: Honoraria. Altman:Fujifilm: Research Funding; Glycomimetics: Other: Data Monitoring Committee; Loxo: Research Funding; Celgene: Research Funding; Boehringer Ingelheim: Research Funding; Astellas: Honoraria, Research Funding; Aptos: Research Funding; Aprea: Research Funding; Amgen: Research Funding; Abbvie: Honoraria, Research Funding; ALX Oncology Inc: Research Funding; Syros: Membership on an entity's Board of Directors or advisory committees; Kura Oncology: Membership on an entity's Board of Directors or advisory committees, Research Funding; Kartos Therapeutics: Research Funding; ImmunoGen: Research Funding; Biosight: Membership on an entity's Board of Directors or advisory committees, Other: reumbursement for travel, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal